The promise of artificial intelligence in medicine is a powerful and captivating narrative, one filled with algorithms that can detect disease before symptoms appear and personalized treatments tailored to an individual’s unique genetic code. Yet, for the clinicians on the front lines, this gleaming high-tech vision stands in stark contrast to the daily, grinding reality of navigating cumbersome digital systems that seem designed to obstruct rather than facilitate patient care. The future of healthcare is not being held back by a lack of advanced algorithms, but by the profoundly unstable and fragmented digital ground upon which they are expected to be built. Before healthcare can leap into the AI era, it must first take a deliberate and critical step back to repair its very foundation.
The AI Paradox Why Isnt Healthcares High-Tech Future Here Yet
A significant chasm exists between the public’s excitement for AI-driven medicine and the frustrating reality of daily clinical practice. The dialogue is dominated by headlines heralding AI models that outperform human specialists in diagnostic imaging or predict patient outcomes with uncanny accuracy. This generates an expectation of imminent, revolutionary change. However, inside hospitals and clinics, healthcare professionals spend hours wrestling with electronic health records that are little more than digitized filing cabinets, manually re-entering data, and chasing down information from other facilities. This disconnect fuels a sense of disillusionment, where the theoretical potential of AI seems light-years away from the practical challenges of delivering care.
The core of this paradox lies in a fundamental question: Is the primary roadblock the AI technology itself, or is it the crumbling digital infrastructure it is meant to operate upon? While research in machine learning and large language models continues to accelerate at an extraordinary pace, these sophisticated tools are data-hungry. They require vast quantities of clean, structured, and interoperable data to function effectively and safely. The current healthcare ecosystem, characterized by information silos and a reliance on unstructured, narrative-based notes, cannot provide this fuel. Consequently, the most brilliant AI algorithms remain stuck in research labs, unable to be deployed at scale because the foundational plumbing of healthcare data is simply not connected.
This situation creates a precarious scenario where investment and attention are disproportionately focused on the most advanced applications of AI while the fundamental enabling layer is neglected. It is akin to designing a high-performance engine for a car that has no chassis, wheels, or fuel line. Without a robust digital framework that prioritizes data quality, accessibility, and security, the AI revolution in healthcare will remain a paradox—a future that is always just over the horizon but never quite arrives. The industry must shift its focus from the glittering endpoint of AI to the meticulous, and arguably more critical, task of building the digital roads required to get there.
The Digital Mirage How Healthcares Tech Revolution Stalled
The initial promise of digital tools in healthcare was one of liberation and efficiency. Electronic Health Records (EHRs) were introduced with the goal of replacing cumbersome paper charts, streamlining workflows, and creating a unified source of patient information. In practice, however, many of these systems have had the opposite effect. Instead of alleviating administrative burdens, they have often amplified them. Clinicians report spending a significant portion of their day on data entry, clicking through poorly designed user interfaces, and navigating non-intuitive menus. These systems, frequently designed without meaningful clinical input, have become a primary source of professional burnout, transforming the practice of medicine into an exercise in clerical work.
This poor design has turned highly trained professionals into “manual integrators” of information. In a fragmented digital landscape where a patient’s data is scattered across different hospitals, specialist clinics, and pharmacies, the responsibility for piecing together a coherent medical history falls squarely on the clinician. An EHR in one hospital cannot seamlessly communicate with a system in another, forcing doctors to rely on faxes, phone calls, and patient memory to fill in dangerous gaps. This manual integration is not only inefficient and prone to error but also represents a colossal failure of the digital promise. The technology, meant to connect and clarify, has instead created new walls and increased cognitive load on the very people it was intended to support.
From the patient’s perspective, this digital mirage fosters deep-seated concerns about data privacy and security. The fragmented nature of the system means their sensitive health information is stored in numerous, disconnected databases, each with its own vulnerabilities. High-profile data breaches have eroded public trust, making patients hesitant to fully embrace digital health tools. Their experience is often one of inconvenience, where they are repeatedly asked for the same information at every new touchpoint in the healthcare system. This lack of a unified, secure, and patient-centric digital identity undermines both the efficiency of care and the fundamental relationship of trust between patients and the healthcare system.
The Anatomy of a Broken System Identifying the Core Foundational Cracks
At the heart of healthcare’s digital dysfunction is a profound data disconnect. Clinical communication relies heavily on narrative—the detailed stories, observations, and reasoning that clinicians record to care for their patients. This unstructured text is rich with context and nuance, essential for human-to-human understanding. However, this same data is largely opaque to machines. Artificial intelligence, particularly machine learning, thrives on structured, codifiable data—discrete values entered into specific fields, such as a blood pressure reading, a diagnosis code, or a medication dosage. The failure of current systems to bridge this gap, to intelligently capture structured data from clinical narratives without disrupting workflow, is a primary reason why valuable health information remains locked away and unusable for large-scale analysis.
Compounding this issue is the enduring interoperability crisis. The term refers to the inability of different health information systems to communicate and exchange data seamlessly. In the current environment, a patient’s health record is not a single, portable entity but a collection of isolated fragments held by various providers. This creates dangerous information silos. A primary care physician may be unaware of a critical test result from a specialist, or an emergency room doctor might not have access to a patient’s list of allergies from their regular pharmacy. This lack of a holistic view not only leads to redundant testing and increased costs but also poses a direct threat to patient safety. True interoperability is not a technical luxury; it is a clinical necessity for ensuring continuity and quality of care.
Ultimately, these problems are symptoms of a deeper, systemic flaw: the prevalence of a “technology-first” design philosophy. For decades, digital health tools have been developed by engineers with limited input from the people who would use them every day. The focus has been on technical specifications and billing requirements rather than on the real-world workflows of clinicians, nurses, and other healthcare staff. This approach has resulted in products that are powerful in theory but clumsy and counterintuitive in practice. A sustainable digital transformation requires a fundamental reversal of this model, placing the needs and insights of end-users—including patients—at the very center of the design and development process.
A New Blueprint Expert Consensus on a Human-Centered Digital Transformation
An emerging consensus among health-tech experts and clinical leaders underscores a foundational imperative: the digital revolution must fully precede the AI revolution. Attempting to layer sophisticated AI onto a broken digital infrastructure is not just inefficient; it is potentially unsafe. The focus, therefore, must shift toward building a robust, reliable, and user-friendly digital ecosystem first. This involves prioritizing the systematic collection of high-quality, structured data and ensuring that systems are truly interoperable. Only when data can flow freely and securely across the entire care continuum can AI tools be deployed responsibly to analyze that data and generate meaningful insights. This foundational work is the essential, non-negotiable prerequisite for realizing the promise of AI in medicine.
This new blueprint for digital transformation is anchored in the power of co-creation and Service Design. This represents a radical departure from the traditional top-down, technology-first approach. In a co-creation model, multidisciplinary teams comprising clinicians, nurses, patients, software developers, and system designers work collaboratively throughout the entire lifecycle of a tool, from initial concept to final implementation and iteration. By embedding end-users in the development process, the resulting technologies are far more likely to be clinically relevant, intuitive to use, and seamlessly integrated into existing workflows. Patients, in particular, offer invaluable insights from their lived experiences, ensuring that tools designed for self-management or remote monitoring are practical, engaging, and genuinely supportive of their health goals.
Further enhancing this human-centered approach is the integration of insights from behavioral science. Designing a tool that is merely functional is not enough; it must also effectively motivate users toward desired behaviors. Frameworks like the Capability, Opportunity, Motivation, and Behavior (COM-B) model provide a systematic way to understand and address the factors that influence human actions. By applying these principles, digital tools can incorporate subtle “nudges” and supportive features that encourage medication adherence, promote healthier lifestyle choices, and guide clinicians toward best practices. For instance, an mHealth app for managing a chronic condition could be designed to deliver personalized reminders and positive reinforcement, making it easier for patients to stick to their treatment plans and achieve better health outcomes. This fusion of technology, clinical expertise, and behavioral science is key to creating digital tools that not only work but also drive meaningful change.
The Path Forward A Practical Framework for Building a Future-Ready Foundation
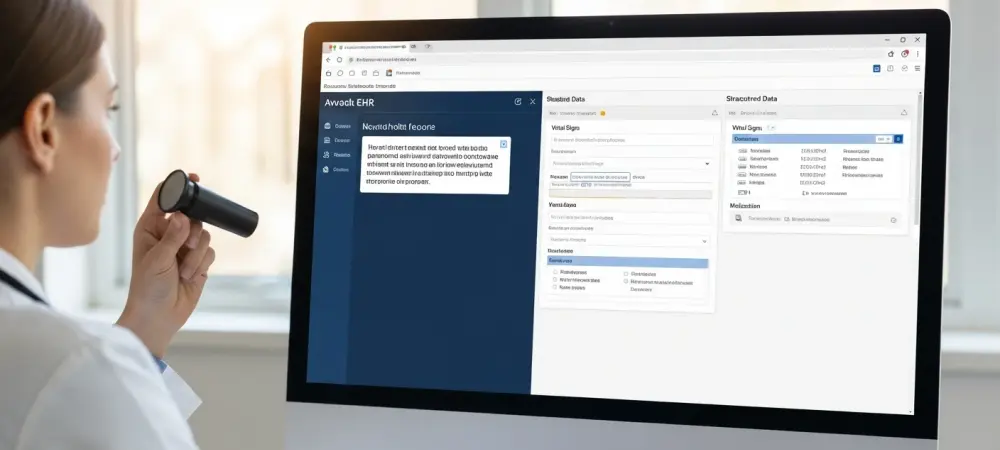
The first practical step toward a future-ready foundation is to systematize the capture of structured data. This does not mean forcing clinicians to abandon narrative notes, which are vital for nuanced communication. Instead, it requires designing intelligent systems that work in the background. An ideal EHR would allow a physician to type or dictate their clinical assessment naturally while the system uses natural language processing to identify and codify key concepts—such as diagnoses, symptoms, and medications—using standardized terminologies like SNOMED-CT and LOINC. This dual approach preserves the richness of human narrative for patient care while simultaneously generating the clean, machine-readable data needed for secondary uses like research, public health surveillance, and training AI models.
Next, achieving true interoperability must be elevated from a desirable feature to a non-negotiable, mandated standard for all health technology systems. Seamless and secure data exchange should be a core requirement for any digital tool used in healthcare. This ensures that a patient’s complete medical history is available to authorized providers at the point of care, regardless of where that care is delivered. Establishing and enforcing robust interoperability standards, such as Fast Healthcare Interoperability Resources (FHIR), is critical for breaking down information silos. This not only improves patient safety and care coordination but also enables the aggregation of large, diverse datasets essential for population health management and the advancement of medical research.
Finally, this new model must be piloted and proven in a “living lab”—a real-world clinical setting that can test and refine these principles. A complex specialty like nephrology provides an ideal environment. Here, a co-created mHealth app could be deployed for remote monitoring of patients on home dialysis, using real-time data to prevent complications. The vast datasets generated from dialysis treatments across a network of clinics could be leveraged to train predictive machine learning models that identify patients at high risk of adverse events. Furthermore, specialized EHR modules could be developed to automatically populate registries for rare kidney diseases, capturing research-grade data during routine clinical encounters. By demonstrating tangible success in a challenging field, this framework can provide a validated blueprint for a nationwide, human-centered digital transformation.
The journey toward an AI-powered healthcare system was understood not as a single technological leap but as a methodical process of construction. The initial excitement had been tempered by the pragmatic realization that no advanced intelligence, artificial or otherwise, could function effectively amidst chaos. The critical work involved laying down the foundational elements of a truly digital health ecosystem: user-centric design principles were embraced, interoperability standards were enforced, and data was treated as a precious asset to be structured and shared responsibly. By focusing on fixing the present, healthcare professionals and technologists together built the stable platform upon which a more intelligent and equitable future of medicine could finally be realized.