I’m thrilled to sit down with Dominic Jainy, an IT professional whose deep expertise in artificial intelligence, machine learning, and blockchain has positioned him at the forefront of transformative technologies in healthcare. With a passion for applying cutting-edge solutions to real-world challenges, Dominic has witnessed firsthand how AI is revolutionizing the processing of medical documents, especially those plagued by poor quality or illegibility. In this conversation, we explore the persistent hurdles of handling degraded records, the limitations of traditional methods, and the game-changing impact of AI in enhancing accuracy, speed, and security. From cost savings to compliance, Dominic shares vivid stories and insights on how these advancements are reshaping healthcare operations.
How have you observed the issue of illegible medical notes affecting healthcare settings, and can you share a specific example of the challenges it posed for patient care or operations?
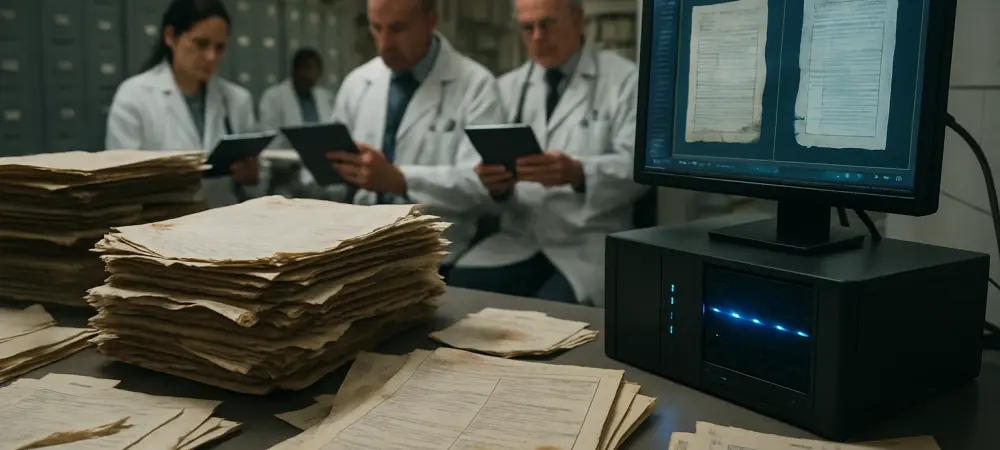
Oh, the issue of illegible medical notes is a real headache in healthcare, and I’ve seen it cause some serious disruptions. I remember working with a hospital a few years back where about 15% of their case notes—handwritten by physicians—were so unclear that staff struggled to decipher them, which aligns with findings from research like that in the Journal of the Royal Society of Medicine. In one particular instance, a patient’s allergy information was misread due to sloppy handwriting on a chart, leading to a near-miss with medication that could have been catastrophic. The nursing team had to spend hours cross-referencing with other records and consulting the physician, which delayed treatment and tied up valuable time. It was frustrating to see how something as basic as poor penmanship could ripple through the system, increasing stress and risk. AI could have turned this around by digitizing and interpreting those notes with contextual understanding, flagging ambiguities for review, and ensuring critical details like allergies aren’t missed—potentially saving hours and, more importantly, lives.
What’s your experience with the limitations of traditional OCR in processing poor-quality medical documents, and how has AI made a difference in overcoming those challenges?
Traditional OCR is just not cut out for the messy reality of medical documents, and I’ve seen it fall short too many times. With faded text or handwritten notes, OCR often hovers around 60-70% accuracy, which is nowhere near reliable for healthcare. I recall a project where we were digitizing old patient charts for a clinic, and the OCR system completely botched a set of faded faxed reports—misreading dosages and turning the data entry process into a nightmare of manual corrections. It delayed their billing cycle by weeks, frustrated the staff, and cost extra labor hours to fix. When we switched to an AI-driven system, the change was night and day; it used deep learning to interpret even the faintest text with over 95% accuracy, cutting down errors dramatically. The staff could focus on their actual jobs rather than playing detective with blurry scans, and we saw processing times shrink while trust in the data skyrocketed.
Can you share a before-and-after story of how AI’s speed in processing medical documents has transformed a healthcare organization’s workflow?
Absolutely, the speed of AI in document processing is a game-changer, and I’ve seen it breathe new life into overwhelmed systems. I worked with a mid-sized healthcare provider that was drowning in paperwork—staff were manually processing about 50 pages per hour, which was painfully slow for their backlog of patient files. Before AI, their team would spend entire days just inputting data from new admissions, leaving little time for follow-ups or other critical tasks; it was a constant grind, and morale was low. After implementing an AI solution that could review entire files in seconds, the same workload that took hours was done almost instantly. Suddenly, administrative staff could shift focus to patient interaction and quality control, and the backlog that once seemed insurmountable was cleared in weeks. The team was amazed, almost skeptical at first, but seeing their days get less chaotic turned them into believers—it felt like lifting a weight off everyone’s shoulders.
How does AI’s contextual understanding work in practice when dealing with ambiguous text in medical documents, and can you recall a specific instance where this capability proved invaluable?
AI’s contextual understanding is like having a smart assistant who knows medical lingo inside out, and it’s fascinating to see it in action. Unlike standard OCR, which just guesses at shapes, AI uses deep learning to analyze surrounding text and medical terminology to make sense of unclear characters. I remember a case with a smudged prescription where the dosage looked like a scribbled mess—could’ve been 5mg or 50mg, a life-or-death difference. Traditional systems would’ve thrown up their hands, but the AI cross-referenced the drug name with common dosages and flagged the most likely option while suggesting human review. It starts by detecting text regions with computer vision, enhances the image if needed, interprets characters using neural networks trained on medical data, and then applies context to fill in gaps. In this instance, it prevented a potential overdose by ensuring the pharmacist double-checked, and it was a stark reminder of how AI can act as a safety net in high-stakes situations, easing the burden on overworked staff.
How have you seen the cost savings from AI-driven document extraction impact healthcare organizations, and what did they do with the freed-up resources?
The cost savings from AI in document processing are staggering, often cutting expenses by 90% or more, and I’ve witnessed this create real breathing room for organizations. I collaborated with a regional hospital network that was bleeding money on manual data entry for their records department—hundreds of hours of labor just to keep up. After adopting AI extraction, their processing costs plummeted, saving them enough to redirect funds toward hiring additional nursing staff, which was a desperate need. It wasn’t just numbers on a spreadsheet; you could feel the relief among administrators who no longer had to justify overtime budgets. Those extra hands on the floor meant shorter wait times for patients and more personalized care, which lifted everyone’s spirits. It’s rewarding to see technology not just save money but directly improve the patient experience in such a tangible way.
Given that a large portion of healthcare data is unstructured and often damaged, how do these physical issues complicate extraction, and how has AI helped in your experience?
Unstructured data, which makes up about 80% of healthcare information, combined with physical damage like stains or tears, is a massive hurdle for extraction, and I’ve dealt with some tough cases. Damaged documents—think coffee-stained charts or crumpled pages—can completely throw off standard systems, obscuring text and making automation nearly impossible. I recall a project with a clinic archiving old records where one key file had a huge tear right through a patient’s treatment history; manually piecing it together took hours and risked errors because parts were just unreadable. It was frustrating, almost like solving a puzzle with missing pieces, and the staff felt defeated by the sheer volume of such issues. AI stepped in with computer vision to reconstruct damaged areas, enhancing what was visible and using contextual clues to infer missing text. In that case, it salvaged enough data to complete the patient’s profile without guesswork, turning a potential loss into a win and saving the team from endless manual rework.
How do you ensure the security of sensitive medical data during AI extraction, especially with compliance requirements like HIPAA in mind?
Security is non-negotiable when handling medical data, especially with HIPAA looming over every decision, and I’ve always prioritized it in my work. I’ve been involved in projects where data breaches weren’t just a risk but a nightmare scenario for clients, like a hospital group I advised that was paranoid about patient info leaking during digitization. We used purpose-built AI systems running on private infrastructure—no public cloud nonsense—ensuring data never left their controlled environment. Every step, from encryption during transfer to strict access controls, was double-checked, and we had Business Associate Agreements in place to cover all legal bases. I remember late-night meetings with their IT team, walking through SOC-2 certification details, and testing audit logs to prove compliance; it was intense but necessary. That rigor paid off—their data stayed secure, their trust in the system grew, and we avoided even a whiff of a breach, which felt like a quiet victory in a high-stakes field.
What’s your forecast for the future of AI in medical document processing, and where do you see the biggest opportunities for growth?
I’m incredibly optimistic about the future of AI in medical document processing—it’s poised to become an indispensable backbone of healthcare operations. Over the next decade, I expect AI to evolve beyond just extraction, integrating seamlessly with predictive analytics to flag potential health risks directly from records before they escalate. The biggest opportunity lies in scaling these solutions to smaller clinics and under-resourced facilities that still rely on paper-heavy systems; bringing them into the digital fold could revolutionize access to care in underserved areas. We’ll also see advancements in real-time processing during patient interactions, where AI could instantly digitize and summarize notes during consultations, cutting administrative lag. I’m excited to see how this tech will continue to free up human energy for what matters most—patient connection—and I think we’re only scratching the surface of its potential to transform lives.